If you’re considering drug rehabilitation in Ohio, understanding your insurance options is crucial. Thanks to federal regulations like the Mental Health Parity and Addiction Equity Act (MHPAEA), many insurance plans are required to provide comparable coverage for addiction treatment as they do for other medical conditions.
In this article, you can find information on insurance plans that cover drug and alcohol addiction treatment, as well as the benefits you can get.
Insurance Coverage in Ohio for Substance Use Treatment
When seeking help for substance use disorders, having insurance coverage for drug and alcohol use can significantly ease the financial burden of the cost of treatment. In Ohio, addiction treatment options are more accessible when you have a good insurance provider.
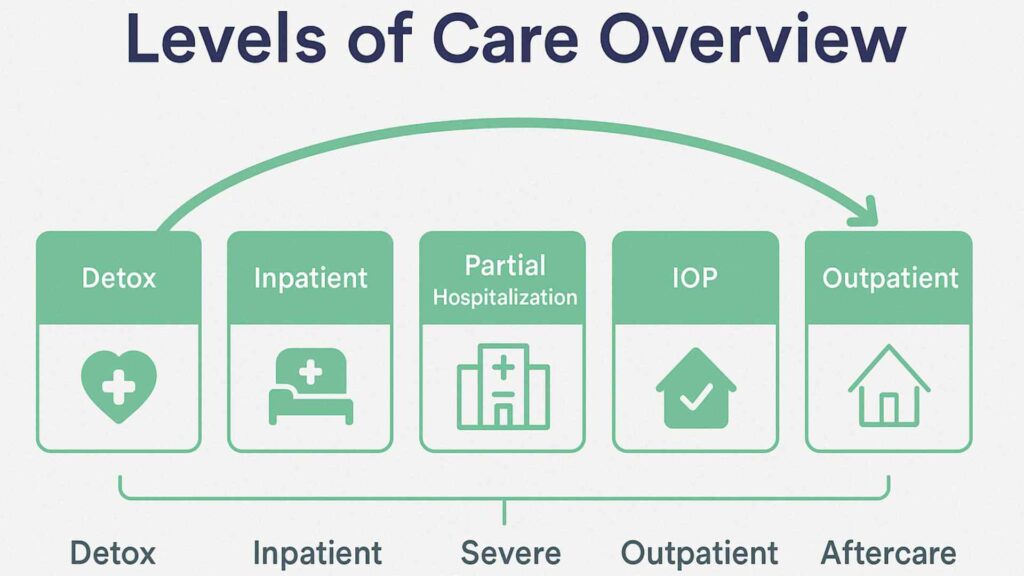
Many rehab programs accept various insurance plans, ensuring that you can find the right fit for your needs without overwhelming costs. It’s crucial to understand that your insurance coverage typically includes treatment for substance abuse, which can encompass inpatient and outpatient services, detoxification, and aftercare.
Types of Insurance Plans Covering Drug Rehab in Ohio and What Services Are Covered
Under federal laws like the ACA and the Mental Health Parity and Addiction Equity Act, insurers must provide coverage for addiction treatment that’s comparable to other medical services. You shouldn’t face higher costs for pre-existing conditions, and there’s no lifetime limit on benefits.
Many insurance plans, especially those from Marketplace health insurance providers, are required to cover substance abuse treatment in rehab facilities as essential benefits. This includes therapy, counseling, and extensive coverage for substance abuse, including inpatient and outpatient treatment, without denying pre-existing conditions.
Medicaid is another option, offering crucial access to treatment for those in need.
Private insurance and employer-sponsored insurance policies may also include behavioral health treatment, though you’ll have to verify your insurance coverage.
Services typically covered include detoxification from drugs or alcohol, medication-assisted treatment, and aftercare programs at addiction treatment centers.
Insurance Providers Known to Cover Drug Rehab Services in Ohio
Medicaid
Ohio Medicaid covers a wide range of substance abuse treatment services, including outpatient and inpatient treatment, medication-assisted treatment, and counseling. Coverage specifics may vary, but Medicaid is a major payer for addiction treatment in Ohio.
Anthem Blue Cross Blue Shield (BCBS)
Anthem BCBS plans, including those purchased through the Health Insurance Marketplace and employer-sponsored policies, are required by the Affordable Care Act (ACA) to cover addiction treatment as an essential health benefit. Many Ohio rehab centers accept Anthem BCBS, but coverage details such as copays, deductibles, and in-network providers depend on your specific plan.
Aetna
Aetna insurance plans are accepted by several Ohio rehab centers. Coverage typically includes detox, inpatient, outpatient, and medication-assisted treatment, subject to insurance verification and pre-authorization requirements.
United Healthcare
United Healthcare is another major insurer whose plans are accepted by Ohio treatment facilities. These plans often cover treatment for substance use disorders as well as a full spectrum of rehab services, including detox, residential, and outpatient care.
Medical Mutual
Medical Mutual, a prominent Ohio-based insurer, offers plans that cover drug and alcohol rehab services. Coverage includes inpatient and outpatient programs, but specifics depend on the policy and provider network.
Accessing Substance Abuse Treatment Services in Ohio Using Your Health Insurance Plan
Finding certified treatment centers in Ohio that accept health insurance policies that cover rehab is a critical step in your recovery. The state has numerous accredited facilities equipped to treat various substance use disorders, many of which work with major insurance providers to cover the cost of treatment.
Features of Certified Treatment Facilities
Addiction treatment programs are led by licensed medical professionals and experienced addiction specialists who provide compassionate, expert care. They utilize evidence-based treatment methods to ensure the highest standard of effectiveness and safety.
Patients have access to multiple levels of care, including detoxification, inpatient rehabilitation, and outpatient services, allowing for a personalized recovery journey. For those facing co-occurring mental health conditions, the alcohol rehab centers also offer dual diagnosis treatment to address both addiction and underlying psychological disorders.
Rehab insurance coverage should also include 24/7 care services that are vital to effective addiction treatment. These are emergency medical interventions and crisis management support to ensure immediate and appropriate responses during critical moments.
Around-the-clock care also includes immediate intake assessments to streamline the admission process and provide timely care. Continuous monitoring during detox is typically part of the coverage, ensuring patient safety and stability throughout the withdrawal phase. In addition, on-call medical staff are available at all hours to address any urgent needs, providing a constant layer of professional support throughout the recovery journey.
All services are delivered in full compliance with state and federal regulations, ensuring quality and accountability every step of the way.
Treatment centers maintain relationships with insurers to streamline authorization processes, allowing you to focus on recovery rather than administrative hurdles.
Parity Protections and Legal Requirements
Insurance plans in Ohio are designed to ensure that individuals seeking treatment for substance use disorders aren’t unfairly burdened compared to those seeking medical or surgical care.
Parity protections require insurance plans to offer substance abuse treatment benefits that are equal to medical coverage. This means that financial limits, such as deductibles and copays, must be on par. Treatment limitations, including the number of visits or required pre-authorization, should be consistent across both types of care.
By enforcing these legal requirements, insurance companies must provide comprehensive health insurance benefits, ensuring adequate addiction treatment coverage.
Understanding these protections helps you navigate your options, making it easier to access the necessary coverage for mental health and substance use treatment in Ohio. Again, it’s important to check with your insurance company to find out which treatments are covered by your insurance plan.
Final Thoughts from Abundance Treatment
Whether you have Marketplace, Medicaid, or a private plan, it’s essential to understand your benefits. Remember, federal parity laws ensure you get fair access to addiction services.
At Abundance Treatment, we proudly accept insurance coverage for drug rehab, working closely with providers to make high-quality, compassionate treatment in Ohio accessible and affordable for those ready to take the first step toward lasting recovery.